What Are The Causes Of Severs Disease?
Severs disease is pain in one or both heels when walking. The pain comes from the area between the sections of bone that make up the heel. As you go through a ?growth spurt? the tendon at the back of the heel (Achilles tendon) pulls at the heel bone. This makes you limp or walk on your toes and often creates a lump on your heel. The reason the tendon is tight is because your bones grow faster than your muscles. It usually affects boys between eight to ten years old, girls between ten and 12 years old, children in a ?growth spurt?, children involved in sports, usually those that involve running and jumping.
Causes
Sever's disease usually develops as a result of overuse and is common in active children between the ages of 8 to 12. Activities that involve running or jumping can cause undue stress on the calcaneal apophysis. This in turn leads to the development of microscopic damage to the calcaneal apophysis resulting in inflammation and pain. Poor flexibility of the calf muscles and of the Achilles tendon, overpronation (feet rolled in) and inappropriate footwear are some of the other factors that can cause Sever's disease.
Symptoms
The typical patient is a child between 10 and 13 years of age, complaining of pain in one or both heels with running and walking. The pain is localized to the point of the heel where the tendo-achilles inserts into the calcaneus (heel bone), and is tender to deep pressure at that site. Walking on his toes relieves the pain.
Diagnosis
Low-grade inflammation of the calcaneal apophysis cannot be seen on x-ray. Therefore, although x-rays are often done to rule out bony injuries in children with Sever's disease these x-rays are usually normal. Advanced Sever's disease can be seen on x-ray but usually the problem is treated before it reaches this point. Other diagnostic tests, such as bone scans or MRI's, are not usually required in typical cases of Sever's disease. These, or other tests, may be required to rule out other conditions, such as stress fractures of the calcaneus or other bony abnormalities that can mimic Severs disease.
Non Surgical Treatment
The immediate goal of treatment is pain relief. Because symptoms generally worsen with activity, the main treatment for Sever's disease is rest, which helps to relieve pressure on the heel bone, decreasing swelling and reducing pain. As directed by the doctor, a child should cut down on or avoid all activities that cause pain until all symptoms are gone, especially running barefoot or on hard surfaces because hard impact on the feet can worsen pain and inflammation. The child might be able to do things that do not put pressure on the heel, such as swimming and biking, but check with a doctor first. The doctor might also recommend that a child with Sever's disease perform foot and leg exercises to stretch and strengthen the leg muscles and tendons, elevate and apply ice (wrapped in a towel, not applied directly to the skin) to the injured heel for 20 minutes two or three times per day, even on days when the pain is not that bad, to help reduce swelling, use an elastic wrap or compression stocking that is designed to help decrease pain and swelling, take an over-the-counter medicine to reduce pain and swelling, such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin). Children should not be given aspirin for pain due to the risk of a very serious illness called Reye syndrome. In very severe cases, the doctor might recommend that the child wear a cast for anywhere from 2 to 12 weeks to immobilize the foot so that it can heal.
Exercise
Exercises that help to stretch the calf muscles and hamstrings are effective at treating Sever's disease. An exercise known as foot curling, in which the foot is pointed away from the body, then curled toward the body in order to help stretch the muscles, has also proven to be very effective at treating Sever's disease. The curling exercise should be done in sets of 10 or 20 repetitions, and repeated several times throughout the day.
Causes And Treatment
Overview
A painful flat foot, or adult acquired flatfoot deformity, is a progressive collapsing of the arch of the foot that occurs as the posterior tibial tendon becomes insufficient due to various factors. Early stages may present with only pain along the posterior tibial tendon whereas advanced deformity usually results in arthritis and rigidity of the rearfoot and ankle. 
Causes
The posterior tibial tendon, which connects the bones inside the foot to the calf, is responsible for supporting the foot during movement and holding up the arch. Gradual stretching and tearing of the posterior tibial tendon can cause failure of the ligaments in the arch. Without support, the bones in the feet fall out of normal position, rolling the foot inward. The foot's arch will collapse completely over time, resulting in adult acquired flatfoot. The ligaments and tendons holding up the arch can lose elasticity and strength as a result of aging. Obesity, diabetes, and hypertension can increase the risk of developing this condition. Adult acquired flatfoot is seen more often in women than in men and in those 40 or older.
Symptoms
Pain along the inside of the foot and ankle, where the tendon lies. This may or may not be associated with swelling in the area. Pain that is worse with activity. High-intensity or high-impact activities, such as running, can be very difficult. Some patients can have trouble walking or standing for a long time. Pain on the outside of the ankle. When the foot collapses, the heel bone may shift to a new position outwards. This can put pressure on the outside ankle bone. The same type of pain is found in arthritis in the back of the foot. Asymmetrical collapsing of the medial arch on the affected side.
Diagnosis
Observe forefoot to hindfoot alignment. Do this with the patient sitting and the heel in neutral, and also with the patient standing. I like to put blocks under the forefoot with the heel in neutral to see how much forefoot correction is necessary to help hold the hindfoot position. One last note is to check all joints for stiffness. In cases of prolonged PTTD or coalition, rigid deformity is present and one must carefully check the joints of the midfoot and hindfoot for stiffness and arthritis in the surgical pre-planning.
Non surgical Treatment
Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery and progression of your condition can be arrested. In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle, and increasing limitations on walking, running, or other activities. In many cases of PTTD, treatment can begin with non-surgical approaches that may include. Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may provide you with an ankle brace or a custom orthotic device that fits into the shoe. Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weight-bearing for a while. Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Shoe modifications. Your foot and ankle surgeon may advise changes to make with your shoes and may provide special inserts designed to improve arch support. 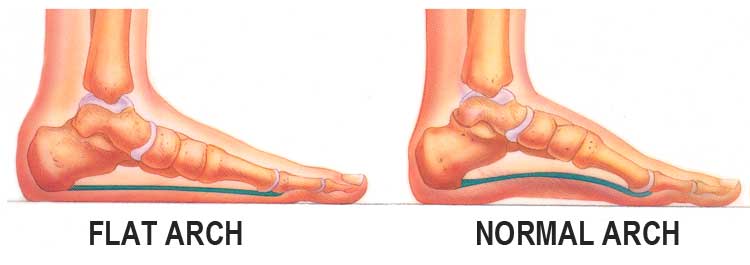
Surgical Treatment
For more chronic flatfoot pain, surgical intervention may be the best option. Barring other serious medical ailments, surgery is a good alternative for patients with a serious problem. There are two surgical options depending on a person?s physical condition, age and lifestyle. The first type of surgery involves repair of the PTT by transferring of a nearby tendon to help re-establish an arch and straighten out the foot. After this surgery, patients wear a non-weight bearing support boot for four to six weeks. The other surgery involves fusing of two or three bones in the hind foot below the ankle. While providing significant pain relief, this option does take away some hind foot side-to-side motion. Following surgery, patients are in a cast for three months. Surgery is an effective treatment to address adult-acquired flatfoot, but it can sometimes be avoided if foot issues are resolved early. That is why it is so important to seek help right away if you are feeling ankle pain. But perhaps the best way to keep from becoming flatfooted is to avoid the risk factors altogether. This means keeping your blood pressure, weight and diabetes in check.
What Are The Causes Of Heel Pain

Heel pain is a common foot condition. It's usually felt as an intense pain when using the affected heel. Heel Pain usually builds up gradually and gets worse over time. The pain is often severe and occurs when you place weight on the heel. In most cases, only one heel is affected, although estimates suggest that around a third of people have pain in both heels. The pain is usually worse first thing in the morning, or when you first take a step after a period of inactivity. Walking usually improves the pain, but it often gets worse again after walking or standing for a long time. Some people may limp or develop an abnormal walking style as they try to avoid placing weight on the affected heel.
Causes
There is no one cause of heel pain. Whole text books have been written on Disorders of the Heel. Some of the types of problems that can be seen in the heel include Heel spurs, these are small bony spurs that often develop on the bottom of the heel. They do not really cause any problems. It is only mentioned here as it is a common myth that they are a problem - almost always the pain associated with heel spurs is really plantar fasciitis. Plantar fasciitis is the most common cause of heel pain and is due to a strain of the long ligament along the bottom of the foot. The most symptom is pain when getting out of bed first thing in the morning ('post-static dyskinesia') A number of disease processes can uncommonly cause heel pain, such as rheumatoid arthritis, ankylosing spondylitis and gout. Stress fractures, which is an abnormal reaction of bone to stress can occur in those that are very active (eg athletes) or have weaker bones (eg osteoporosis) Pain at the back of the heel could be due to a number of problems, there could be a bursitis at the back of the heel bone (sometimes called 'Haglund's) there could be problems with the insertion of the achilles tendon, such as tendonitis or calcification. A 'stone' bruise is sometimes considered to be a cause of heel pain, its is simply a bruise of the bone. Another cause of heel pain is problems in the calf muscles that refer pain to the heel (myofascial trigger points) or pain referred from the lower back via the nerves from the back to the heel. Heel pain in children is usually due to severs disease or calcaneal apophysitis.
Symptoms
Initially, this pain may only be present when first standing up after sleeping or sitting. As you walk around, the muscle and tendon loosen and the pain goes away. As this problem progresses, the pain can be present with all standing and walking. You may notice a knot or bump on the back of the heel. Swelling may develop. In some cases, pressure from the back of the shoe causes pain.
Diagnosis
Your GP or podiatrist (a healthcare professional who specialises in foot care) may be able to diagnose the cause of your heel pain by asking about your symptoms and examining your heel and foot. You will usually only need further tests if you have additional symptoms that suggest the cause of your heel pain is not inflammation, such as numbness or a tingling sensation in your foot - this could be a sign of nerve damage in your feet and legs (peripheral neuropathy), your foot feels hot and you have a high temperature (fever) of 38C (100.4F) or above - these could be signs of a bone infection, you have stiffness and swelling in your heel - this could be a sign of arthritis. Possible further tests may include, blood tests, X-rays - where small doses of radiation are used to detect problems with your bones and tissues, a magnetic resonance imaging (MRI) scan or ultrasound scan, which are more detailed scans.
Non Surgical Treatment
Depending on the underlying cause, treatment can include. Rest from activities that stress the heel (such as running and jumping). Ice packs. Regular foot massage, concentrating on the arch of the foot. Professional strapping. A splint worn at night. Flexibility exercises. Ultrasound therapy. Anti-inflammatory medicine (topical or oral). Checking your posture and walking style, to correct imbalances and gait abnormalities that may contribute to the pain. Shoe inserts (orthoses) to help support the foot. In some cases, surgery may be recommended to treat conditions including neuroma, bursitis and heel spurs.
Surgical Treatment
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you. No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
Prevention

The following steps will help prevent plantar fasciitis or help keep the condition from getting worse if you already have it. The primary treatment is rest. Cold packs application to the area for 20 minutes several times a day or after activities give some relief. Over-the-counter pain medications can help manage the pain, consult your healthcare professional. Shoes should be well cushioned, especially in the midsole area, and should have the appropriate arch support. Some will benefit from an orthotic shoe insert, such as a rubber heel pad for cushioning. Orthotics should be used in both shoes, even if only one foot hurts. Going barefoot or wearing slipper puts stress on your feet. Put on supportive shoes as soon as you get out of bed. Calf stretches and stretches using a towel (place the towel under the ball of your feet and pull gently the towel toward you and hold a few seconds) several times a day, especially when first getting up in the morning. Stretching the Achilles tendon at the back of the heel is especially important before sports, but it is helpful for nonathletes as well. Increasing your exercise levels gradually. Staying at a healthy weight. Surgery is very rarely required.
Dealing With Achilles Tendinitis
 The Achilles tendon camera.gif connects the calf muscle to the heel bone. It lets you rise up on your toes and push off when you walk or run. The two main problems are, Achilles tendinopathy. This includes one of two conditions, Tendinitis. This actually means "inflammation of the tendon." But inflammation is rarely the cause of tendon pain. Tendinosis. This refers to tiny tears (microtears) in the tissue in and around the tendon. These tears are caused by overuse. In most cases, Achilles tendon pain is the result of tendinosis, not tendinitis. Some experts now use the term tendinopathy to include both inflammation and microtears. But many doctors may still use the term tendinitis to describe a tendon injury. Problems with the Achilles tendon may seem to happen suddenly. But usually they are the result of many tiny tears in the tendon that have happened over time. Achilles tendinopathy is likely to occur in men older than 30. Most Achilles tendon ruptures occur in people 30 to 50 years old who are recreational athletes ("weekend warriors"). Ruptures can also happen in older adults.
The Achilles tendon camera.gif connects the calf muscle to the heel bone. It lets you rise up on your toes and push off when you walk or run. The two main problems are, Achilles tendinopathy. This includes one of two conditions, Tendinitis. This actually means "inflammation of the tendon." But inflammation is rarely the cause of tendon pain. Tendinosis. This refers to tiny tears (microtears) in the tissue in and around the tendon. These tears are caused by overuse. In most cases, Achilles tendon pain is the result of tendinosis, not tendinitis. Some experts now use the term tendinopathy to include both inflammation and microtears. But many doctors may still use the term tendinitis to describe a tendon injury. Problems with the Achilles tendon may seem to happen suddenly. But usually they are the result of many tiny tears in the tendon that have happened over time. Achilles tendinopathy is likely to occur in men older than 30. Most Achilles tendon ruptures occur in people 30 to 50 years old who are recreational athletes ("weekend warriors"). Ruptures can also happen in older adults.
Causes
Achilles tendonitis most commonly occurs due to repetitive or prolonged activities placing strain on the Achilles tendon. This typically occurs due to excessive walking, running or jumping activities. Occasionally, it may occur suddenly due to a high force going through the Achilles tendon beyond what it can withstand. This may be due to a sudden acceleration or forceful jump. The condition may also occur following a calf or Achilles tear, following a poorly rehabilitated sprained ankle or in patients with poor foot biomechanics or inappropriate footwear. In athletes, this condition is commonly seen in running sports such as marathon, triathlon, football and athletics.
Symptoms
Achilles tendonitis may be felt as a burning pain at the beginning of activity, which gets less during activity and then worsens following activity. The tendon may feel stiff first thing in the morning or at the beginning of exercise. Achilles tendonitis usually causes pain, stiffness, and loss of strength in the affected area. The pain may get worse when you use your Achilles tendon. You may have more pain and stiffness during the night or when you get up in the morning. The area may be tender, red, warm, or swollen if there is inflammation. You may notice a crunchy sound or feeling when you use the tendon.
Diagnosis
Physicians usually pinch your Achilles tendon with their fingers to test for swelling and pain. If the tendon itself is inflamed, your physician may be able to feel warmth and swelling around the tissue, or, in chronic cases, lumps of scar tissue. You will probably be asked to walk around the exam room so your physician can examine your stride. To check for complete rupture of the tendon, your physician may perform the Thompson test. Your physician squeezes your calf; if your Achilles is not torn, the foot will point downward. If your Achilles is torn, the foot will remain in the same position. Should your physician require a closer look, these imaging tests may be performed. X-rays taken from different angles may be used to rule out other problems, such as ankle fractures. MRI (magnetic resonance imaging) uses magnetic waves to create pictures of your ankle that let physicians more clearly look at the tendons surrounding your ankle joint.
Nonsurgical Treatment
Nonsurgical methods include rest and stop doing activities that cause stress to the tendon. Ice the area by applying ice to the tendon for 15 minutes after exercising. Compress the tendon by using an athletic wrap or surgical tape. Elevate your injury. You can reduce swelling by lying down and raising your foot at a level that is above your heart. Stretch your ankles and calf muscles. Take anti-inflammatory medication (e.g.: ibuprofen to reduce swelling). Wear orthotics and running shoes. Take part in physical therapy.

Surgical Treatment
Surgery is an option of last resort. However, if friction between the tendon and its covering sheath makes the sheath thick and fibrous, surgery to remove the fibrous tissue and repair any tears may be the best treatment option.
Prevention
Suggestions to reduce your risk of Achilles tendonitis include, incorporate stretching into your warm-up and cool-down routines, maintain an adequate level of fitness for your sport, avoid dramatic increases in sports training, if you experience pain in your Achilles tendon, rest the area. Trying to ?work through? the pain will only make your injury worse, wear good quality supportive shoes appropriate to your sport. If there is foot deformity or flattening, obtain orthoses, avoid wearing high heels on a regular basis. Maintaining your foot in a ?tiptoe? position shortens your calf muscles and reduces the flexibility of your Achilles tendon. An inflexible Achilles tendon is more susceptible to injury, maintain a normal healthy weight.
What Leads To Pain On The Heel And Ways To Alleviate It

Overview
The plantar fascia (a connective tissue structure) stretches from the toes and ball of the foot, through the arch, and connects to the heel bone in three places: outside, center and inside. Normally it helps the foot spring as it rolls forward. It also provides support for the arch of the foot. The plantar fascia helps keep the foot on track, cutting down on oscillation. When the foot over-pronates (rolls to the inside) the plantar fascia tries to stabilize it and prevent excessive roll. In time, the inside and sometimes center connections are overstressed and pull away from their attachments. The first sign is usually heel pain as you rise in the morning. When you walk around, the pain may subside, only to return the next morning. Inflammation and increased soreness are the results of long-term neglect and continued abuse. A heel bone spur may develop after a long period of injury when there is no support for the heel. The plantar fascia attaches to the heel bone with small fibers. When these become irritated they become inflamed with blood containing white blood cells. Within the white blood cells are osteoblasts which calcify to form bone spurs and calcium deposits. The body is trying to reduce stress on that area by building a bone in the direction of stress. Unfortunately, these foreign substances cause pain and further irritation in the surrounding soft tissue.
Causes
Training on improper, hard and/or irregular surfaces as well as excessive track work in spiked shoes, or steep hill running, can stress the plantar fascia past its limits of elasticity, leading to injury. Finally, failure in the early season to warm up gradually gives the athlete insufficient time for the structures of the foot to re-acclimate and return to a proper fitness level for intensive exercise. Such unprepared and repeated trauma causes microscopic tearing, which may only be detected once full-blown plantar fasciitis and accompanying pain and debilitation have resulted. If the level of damage to the plantar fascia is significant, an inflammatory reaction of the heel bone can produce spike-like projections of new bone, known as heel spurs. Indeed, plantar fasciitis has occasionally been refereed to as heel spur syndrome, though such spurs are not the cause of the initial pain but are instead a further symptom of the problem. While such spurs are sometimes painless, in other cases they cause pain or disability in the athlete, and surgical intervention to remove them may be required. A dull, intermittent pain in the heel is typical, sometimes progressing to a sharp, sustained discomfort. Commonly, pain is worse in the morning or after sitting, later decreasing as the patient begins walking, though standing or walking for long periods usually brings renewal of the pain.
Symptoms
The most obvious symptom of plantar fasciitis is a sharp pain on the bottom of the foot, near the heel. Here are some signals that this pain may be plantar fasciitis. The pain is strongest first thing in the morning but gets better after a few minutes of walking around. The pain is worse after standing for a long time or after getting up from sitting. The pain develops gradually and becomes worse over time. The pain is worse after exercise or activity than it is during activity. It hurts when stretching the foot. It hurts when pressing on the sides of the heel or arch of the foot.
Diagnosis
Your doctor will ask you about the kind of pain you're having, when it occurs and how long you've had it. If you have pain in your heel when you stand up for the first time in the morning, you may have plantar fasciitis. Most people with plantar fasciitis say the pain is like a knife or a pin sticking into the bottom of the foot. After you've been standing for a while, the pain becomes more like a dull ache. If you sit down for any length of time, the sharp pain will come back when you stand up again.
Non Surgical Treatment
Many types of treatment have been used to combat plantar fasciitis, including injections, anti-inflammatory medications, orthotics, taping, manipulation, night splinting, and instrument-assisted soft-tissue manipulation (IASTM). IASTM begins with heat, followed by stretching. Stretching may be enhanced by applying ice to the plantar fascia. These stretches should be performed several times per day, with the calf in the stretched position. IASTM uses stainless-steel instruments to effectively access small areas of the foot. IASTM is believed to cause a secondary trauma to injured soft tissues as part of the healing process. Therapeutic modalities such as low-level laser, ultrasound, and electrical muscular stimulation may be effective in the reduction of pain and inflammation. Low Dye strapping or taping of the foot is an essential part of successful treatment of plantar fasciitis. Extracorporeal shock-wave therapy (ESWT) was introduced with great promise at one time. Recent studies have reported less favorable results. Some report no effect. Previous local steroid injection may actually have a negative effect on results from ESWT.

Surgical Treatment
Surgery for plantar fasciitis can be very successful in the right patients. While there are potential complications, about 70-80% of patients will find relief after plantar fascia release surgery. This may not be perfect, but if plantar fasciitis has been slowing you down for a year or more, it may well be worth these potential risks of surgery. New surgical techniques allow surgery to release the plantar fascia to be performed through small incisions using a tiny camera to locate and cut the plantar fascia. This procedure is called an endoscopic plantar fascia release. Some surgeons are concerned that the endoscopic plantar fascia release procedure increases the risk of damage to the small nerves of the foot. While there is no definitive answer that this endoscopic plantar fascia release is better or worse than a traditional plantar fascia release, most surgeons still prefer the traditional approach.
Prevention
Being overweight can place excess pressure and strain on your feet, particularly on your heels. Losing weight, and maintaining a healthy weight by combining regular exercise with a healthy, balanced diet, can be beneficial for your feet. Wearing appropriate footwear is also important. Ideally, you should wear shoes with a low to moderate heel that supports and cushions your arches and heels. Avoid wearing shoes with no heels.
What Will Cause Plantar Fasciitis To Appear

Overview
Heel pain is most commonly caused by plantar fasciitis, which is the swelling of the tissue that connects the heel bone to the toes at the bottom part of the foot, also known as the plantar fascia. Plantar fasciitis is often described as sharp pain in the middle of the heel, which is typically worse after periods of rest when fascia contracts. The pain usually becomes more bearable as the muscles loosen up during the low-impact walking, but can return even worse after extended periods of walking or standing. The plantar fascia serves as a shock absorber and supports the foot’s arch. Too much tension on the plantar fascia can cause inflammation and swelling. Fortunately in most cases, plantar fasciitis treatment is fairly conservative. Plantar fasciitis exercises, medications and orthotics are usually all that’s needed to manage the pain. Most severe cases may require surgery.
Causes
Plantar fasciitis is the most common injury of the plantar fascia and is the most common cause of heel pain. Approximately 10% of people have plantar fasciitis at some point during their lifetime. It is commonly associated with long periods of standing and is much more prevalent in individuals with excessive inward rolling of the foot, which is seen with flat feet. Among non-athletic populations, plantar fasciitis is associated with obesity and lack of physical exercise.
Symptoms
Plantar fasciitis and heel spur pain usually begins in the bottom of the heel, and frequently radiates into the arch. At times, however, the pain may be felt only in the arch. The pain is most intense when first standing, after any period of rest. Most people with this problem experience their greatest pain in the morning, with the first few steps after sleeping. After several minutes of walking, the pain usually becomes less intense and may disappear completely, only to return later with prolonged walking or standing. If a nerve is irritated due to the swollen plantar fascia, this pain may radiate into the ankle. In the early stages of Plantar Fasciitis and Heel Spurs, the pain will usually subside quickly with getting off of the foot and resting. As the disease progresses, it may take longer periods of time for the pain to subside.
Diagnosis
Your doctor will check your feet and watch you stand and walk. He or she will also ask questions about your past health, including what illnesses or injuries you have had. Your symptoms, such as where the pain is and what time of day your foot hurts most. How active you are and what types of physical activity you do. Your doctor may take an X-ray of your foot if he or she suspects a problem with the bones of your foot, such as a stress fracture.
Non Surgical Treatment
Your GP or podiatrist may advise you to change your footwear. You should avoid wearing flat-soled shoes, because they will not provide your heel with support and could make your heel pain worse. Ideally, you should wear shoes that cushion your heels and provide a good level of support to the arches of your feet. For women wearing high heels, and for men wearing heeled boots or brogues, can provide short- to medium-term pain relief, as they help reduce pressure on the heels. However, these types of shoes may not be suitable in the long term, because they can lead to further episodes of heel pain. Your GP or podiatrist can advise on footwear. Orthoses are insoles that fit inside your shoe to support your foot and help your heel recover. You can buy orthoses off-the-shelf from sports shops and larger pharmacies. Alternatively, your podiatrist should be able to recommend a supplier. If your pain does not respond to treatment and keeps recurring, or if you have an abnormal foot shape or structure, custom-made orthoses are available. These are specifically made to fit the shape of your feet. However, there is currently no evidence to suggest that custom-made orthoses are more effective than those bought off-the-shelf. An alternative to using orthoses is to have your heel strapped with sports strapping (zinc oxide) tape, which helps relieve pressure on your heel. Your GP or podiatrist can teach you how to apply the tape yourself. In some cases, night splints can also be useful. Most people sleep with their toes pointing down, which means tissue inside the heel is squeezed together. Night splints, which look like boots, are designed to keep your toes and feet pointing up while you are asleep. This will stretch both your Achilles tendon and your plantar fascia, which should help speed up your recovery time. Night splints are usually only available from specialist shops and online retailers. Again, your podiatrist should be able to recommend a supplier. If treatment hasn't helped relieve your painful symptoms, your GP may recommend corticosteroid injections. Corticosteroids are a type of medication that have a powerful anti-inflammatory effect. They have to be used sparingly because overuse can cause serious side effects, such as weight gain and high blood pressure (hypertension). As a result, it is usually recommended that no more than three corticosteroid injections are given within a year in any part of the body. Before having a corticosteroid injection, a local anaesthetic may be used to numb your foot so you don't feel any pain.

Surgical Treatment
In cases that do not respond to any conservative treatment, surgical release of the plantar fascia may be considered. Plantar fasciotomy may be performed using open, endoscopic or radiofrequency lesioning techniques. Overall, the success rate of surgical release is 70 to 90 percent in patients with plantar fasciitis. Potential risk factors include flattening of the longitudinal arch and heel hypoesthesia as well as the potential complications associated with rupture of the plantar fascia and complications related to anesthesia.
What Is Pain Under The Heel

Overview
The plantar fascia is a thick band of connective tissue that runs along the underneath of the foot from the heel bone to the toes. At the heel it can also have fascial connections to the achilles tendon. Its job is to maintain the arch of the foot, it acts as a bowstring pulled between the heel and the toes. "Itis" as a suffix indicates inflammation, but with the plantar fascia there is still some controversy over what exactly happens to the tissue when it becomes painful.
Causes
Plantar fasciitis symptoms are usually exacerbated via "traction" (or stretching) forces on the plantar fascia. In simple terms, you plantar fascia is repeatedly overstretched. The most common reason for the overstretching are an elongated arch due to either poor foot biomechanics (eg overpronation) or weakness of your foot arch muscles. Compression type plantar fascia injuries have a traumatic history. Landing on a sharp object that bruises your plantar fascia is your most likely truma. The location of plantar fasciitis pain will be further under your arch than under your heel, which is more likely to be a fat pad contusion if a single trauma caused your pain. The compression type plantar fasciitis can confused with a fat pad contusion that is often described as a "stone bruise".
Symptoms
Plantar fasciitis commonly causes a stabbing pain in the heel of the foot, which is worse during the first few steps of the day after awakening. As you continue to walk on the affected foot, the pain gradually lessens. Usually, only one foot is affected, but it can occur in both feet simultaneously.
Diagnosis
To arrive at a diagnosis, the foot and ankle surgeon will obtain your medical history and examine your foot. Throughout this process the surgeon rules out all the possible causes for your heel pain other than plantar fasciitis. In addition, diagnostic imaging studies such as x-rays or other imaging modalities may be used to distinguish the different types of heel pain. Sometimes heel spurs are found in patients with plantar fasciitis, but these are rarely a source of pain. When they are present, the condition may be diagnosed as plantar fasciitis/heel spur syndrome.
Non Surgical Treatment
Usually, the pain will ease in time. 'Fascia' tissue, like 'ligament' tissue, heals quite slowly. It may take several months or more to go. However, the following treatments may help to speed recovery. A combination of different treatments may help. Collectively, these initial treatments are known as 'conservative' treatments for plantar fasciitis. Rest your foot. This should be done as much as possible. Avoid running, excess walking or standing, and undue stretching of your sole. Gentle walking and exercises described below are fine. Footwear. Do not walk barefoot on hard surfaces. Choose shoes with cushioned heels and a good arch support. A laced sports shoe rather than an open sandal is probably best. Avoid old or worn shoes that may not give a good cushion to your heel. Heel pads and arch supports. You can buy various pads and shoe inserts to cushion the heel and support the arch of your foot. These work best if you put them in your shoes at all times. The aim is to raise your heel by about 1 cm. If your heel is tender, cut a small hole in the heel pad at the site of the tender spot. This means that the tender part of your heel will not touch anything inside your shoe. Place the inserts/pads in both shoes, even if you only have pain in one foot. Pain relief. Painkillers such as paracetamol will often ease the pain. Sometimes anti-inflammatory medicines such as ibuprofen are useful. These are painkillers but also reduce inflammation and may work better than ordinary painkillers. Some people find that rubbing a cream or gel that contains an anti-inflammatory medicine on to their heel is helpful. An ice pack (such as a bag of frozen peas wrapped in a tea towel) held to your foot for 15-20 minutes may also help to relieve pain. Exercises. Regular, gentle stretching of your Achilles tendon and plantar fascia may help to ease your symptoms. This is because most people with plantar fasciitis have a slight tightness of their Achilles tendon. If this is the case, it tends to pull at the back of your heel and has a knock-on effect of keeping your plantar fascia tight. Also, when you are asleep overnight, your plantar fascia tends to tighten up (which is why it is usually most painful first thing in the morning). The aim of these exercises is to loosen up the tendons and fascia gently above and below your heel. Your doctor may refer you to a physiotherapist for exercise guidance.

Surgical Treatment
In unusual cases, surgical intervention is necessary for relief of pain. These should only be employed after non-surgical efforts have been used without relief. Generally, such surgical procedures may be completed on an outpatient basis in less than one hour, using local anesthesia or minimal sedation administrated by a trained anesthesiologist. In such cases, the surgeon may remove or release the injured and inflamed fascia, after a small incision is made in the heel. A surgical procedure may also be undertaken to remove bone spurs, sometimes as part of the same surgery addressing the damaged tissue. A cast may be used to immobilize the foot following surgery and crutches provided in order to allow greater mobility while keeping weight off the recovering foot during healing. After removal of the cast, several weeks of physical therapy can be used to speed recovery, reduce swelling and restore flexibility.